Blue Cross Blue Shield (BCBS), a behemoth in the American healthcare landscape, has long been synonymous with health insurance. With its extensive network and diverse plan offerings, BCBS caters to a wide spectrum of individuals and families, navigating the complexities of healthcare coverage. But with so many plan options and evolving industry trends, understanding the intricacies of BCBS can feel like navigating a labyrinth. This guide dissects the world of BCBS health insurance plans, demystifying key features, coverage benefits, and crucial considerations for consumers.
From the origins of the organization to the latest innovations shaping the future of healthcare, this exploration delves into the nuances of BCBS plans, providing a comprehensive overview for informed decision-making. We’ll examine the different types of plans available, their respective coverage and costs, and the factors that influence premium pricing. Additionally, we’ll shed light on the administrative processes involved in enrollment and claim management, empowering consumers to confidently navigate the world of BCBS health insurance.
BCBS Overview
Blue Cross Blue Shield (BCBS) is a prominent player in the U.S. healthcare insurance market, boasting a rich history and a complex structure. It’s a federation of independent, locally owned and operated companies that provide health insurance to millions of Americans.
History and Role
The first Blue Cross plan was established in 1929 in Baylor University Hospital in Texas. The goal was to provide affordable hospital care to teachers. The concept quickly spread, and by the 1930s, Blue Cross plans were operating in several states. Blue Shield, which focused on physician coverage, emerged in 1939. These two entities eventually merged to form the Blue Cross Blue Shield Association (BCBSA) in 1982.
Today, BCBS is the largest health insurance provider in the United States, covering over 100 million people. It plays a significant role in the healthcare market, providing a wide range of health insurance plans and influencing policy decisions.
Structure of BCBS
BCBS operates through a decentralized structure, with a national association and independent regional affiliates. The BCBSA serves as a coordinating body, providing guidance and support to the affiliates. However, each affiliate is independently owned and operated, setting its own rates, benefits, and policies.
National and Regional Affiliates
There are 36 independent Blue Cross and Blue Shield companies operating across the United States. Each company serves a specific geographic region, with some companies operating in multiple states. This decentralized structure allows BCBS to tailor its plans and services to the specific needs of local communities.
Blue Cross and Blue Shield
“Blue Cross” and ”Blue Shield” are two distinct types of coverage that are often combined under the BCBS umbrella. ”Blue Cross” typically covers hospital services, such as inpatient care, surgery, and emergency room visits. ”Blue Shield” covers physician services, including doctor visits, outpatient care, and mental health services.
“Blue Cross” and ”Blue Shield” are often combined under the BCBS umbrella, providing comprehensive health insurance coverage.
In some regions, ”Blue Cross” and ”Blue Shield” are combined into a single entity, offering both types of coverage under a single plan. However, in other regions, they remain separate entities, offering coverage independently.
Types of BCBS Plans
Blue Cross Blue Shield (BCBS) offers a variety of health insurance plans to meet the needs of different individuals and families. These plans are categorized into different types, each with its own unique features and benefits. Understanding the differences between these plan types can help you choose the one that best suits your individual circumstances and healthcare needs.
Health Maintenance Organization (HMO)
HMOs are known for their lower premiums and cost-sharing, making them a popular choice for budget-conscious individuals. However, they typically have a narrower network of providers and require you to choose a primary care physician (PCP) who will coordinate your care.
- Key Features:
- Lower premiums and co-pays compared to other plans.
- Limited network of providers. You must choose a PCP within the network.
- Typically require a referral from your PCP to see specialists.
- May offer preventive care services with no co-pay.
- Pros:
- Lower monthly premiums and out-of-pocket costs.
- Focus on preventive care and health management.
- Cons:
- Limited network of providers, potentially restricting your choices.
- Need for referrals to see specialists can be inconvenient.
- May not cover out-of-network services, except in emergencies.
Preferred Provider Organization (PPO)
PPOs offer a wider network of providers than HMOs and generally allow you to see specialists without a referral. However, they typically have higher premiums and cost-sharing than HMOs.
- Key Features:
- Larger network of providers compared to HMOs.
- No need for a referral to see specialists.
- Coverage for out-of-network services, but with higher costs.
- Higher premiums and co-pays compared to HMOs.
- Pros:
- More provider options and flexibility in choosing specialists.
- Coverage for out-of-network services, though at a higher cost.
- Cons:
- Higher monthly premiums and out-of-pocket costs.
- Less emphasis on preventive care compared to HMOs.
Exclusive Provider Organization (EPO)
EPOs are similar to HMOs in that they have a limited network of providers and typically require referrals. However, EPOs generally have higher premiums than HMOs and may not cover out-of-network services, even in emergencies.
- Key Features:
- Limited network of providers.
- Typically require a referral from your PCP to see specialists.
- May not cover out-of-network services, even in emergencies.
- Higher premiums compared to HMOs.
- Pros:
- Lower co-pays compared to PPOs.
- May offer lower premiums than PPOs.
- Cons:
- Limited network of providers.
- No out-of-network coverage, even in emergencies.
Point of Service (POS)
POS plans combine elements of HMOs and PPOs. They typically have a network of providers, but you can also see out-of-network providers for an additional cost. POS plans may require referrals for specialists.
- Key Features:
- Combines elements of HMOs and PPOs.
- Offers both in-network and out-of-network coverage.
- May require referrals for specialists.
- Higher premiums than HMOs, but lower than PPOs.
- Pros:
- More flexibility in choosing providers.
- Coverage for both in-network and out-of-network services.
- Cons:
- Higher premiums and co-pays than HMOs.
- May require referrals for specialists.
- Out-of-network services may have higher costs.
Coverage and Benefits
Blue Cross Blue Shield (BCBS) plans typically offer a comprehensive set of health insurance benefits, designed to cover a wide range of medical expenses. These plans often include coverage for medical, dental, vision, and prescription drugs, although the specific benefits and coverage levels may vary depending on the plan.
Understanding Deductibles, Copayments, and Coinsurance
BCBS plans, like many other health insurance plans, employ a system of cost-sharing mechanisms to help manage healthcare costs. This system includes deductibles, copayments, and coinsurance.
- Deductible: This is the amount you pay out-of-pocket for covered healthcare services before your insurance plan begins to pay. For example, if your deductible is $1,000, you would be responsible for the first $1,000 in medical expenses, and your insurance would cover the rest.
- Copayment: This is a fixed amount you pay for specific medical services, such as doctor’s visits or prescription drugs. Copayments are typically a set amount, regardless of the total cost of the service.
- Coinsurance: This is a percentage of the cost of covered healthcare services that you pay after meeting your deductible. For instance, if your coinsurance is 20%, you would pay 20% of the cost of a covered medical procedure after your deductible is met.
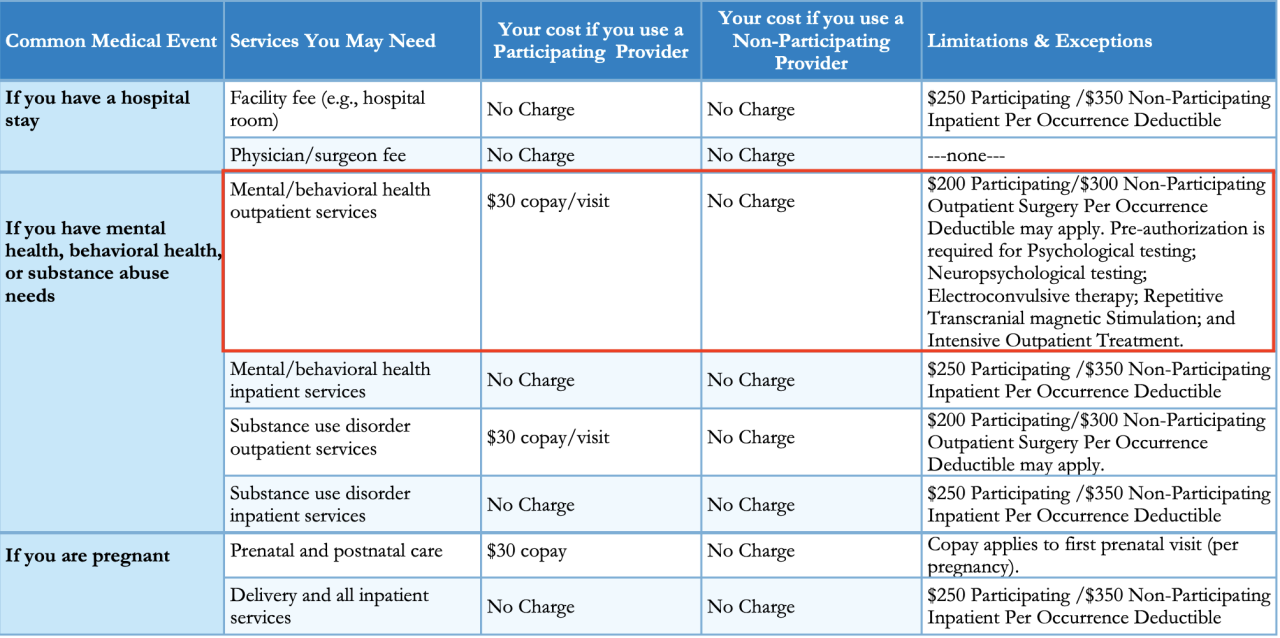
Common Medical Procedures and Services Covered by BCBS Plans
BCBS plans typically cover a wide range of medical procedures and services, including:
- Preventive Care: This includes routine checkups, vaccinations, and screenings for common health conditions.
- Hospitalization: Coverage for inpatient hospital stays, including room and board, nursing care, and medical supplies.
- Surgery: Coverage for surgical procedures, including anesthesia, operating room fees, and post-operative care.
- Physician Services: Coverage for consultations, office visits, and other services provided by doctors.
- Mental Health Services: Coverage for therapy, counseling, and other mental health treatments.
- Prescription Drugs: Coverage for prescription medications, subject to formularies and coverage limitations.
- Emergency Care: Coverage for emergency medical services, including ambulance transportation and treatment in emergency rooms.
Network and Provider Access
Navigating the healthcare system can be complex, and understanding the nuances of network access is crucial when selecting a BCBS health insurance plan. The network refers to the group of doctors, hospitals, and other healthcare providers that have contracted with your insurance company to provide services at a discounted rate. This network access is a key factor in determining the cost of your healthcare and the quality of care you receive.
In-Network and Out-of-Network Providers
When you choose a BCBS plan, you’ll have access to a specific network of healthcare providers. These providers have agreed to accept the negotiated rates set by BCBS. Using providers within your network generally results in lower out-of-pocket costs for you. Conversely, ”out-of-network” providers are those who haven’t contracted with your insurance company. Using these providers typically means higher costs for you.
Network Access Varies by Plan and Location
The size and scope of a BCBS network can vary significantly depending on the specific plan and your geographic location. For example, a plan with a national network might offer access to providers across the country, while a regional plan might have a more limited network within a specific state or region.
Cost and Premiums
Understanding the factors that influence BCBS plan premiums is crucial for making informed decisions about your health insurance coverage. These premiums, which you pay monthly, are determined by various factors, including your age, location, and health status.
Factors Influencing BCBS Plan Premiums
Several factors influence BCBS plan premiums. These include:
- Age: Younger individuals generally pay lower premiums than older individuals, as they tend to have fewer health issues.
- Location: Premiums can vary based on your geographic location. Areas with higher healthcare costs may have higher premiums.
- Health Status: Individuals with pre-existing health conditions may face higher premiums, as they are statistically more likely to utilize healthcare services.
- Plan Type: BCBS offers various plan types, each with its own coverage levels and premium structure.
- Coverage Levels: Higher coverage levels, such as those with lower deductibles and copayments, typically come with higher premiums.
Open Enrollment and BCBS Plan Costs
Open enrollment is a period when individuals can enroll in or change their health insurance plans. This period typically occurs annually. During open enrollment, you can choose a different BCBS plan or switch to a different insurance provider altogether. Changes made during open enrollment typically take effect at the beginning of the next coverage year.
Examples of BCBS Plan Premium Variations
BCBS plan premiums can vary significantly based on the plan type and coverage levels. Here are some examples:
- Bronze Plans: These plans typically have the lowest premiums but also have the highest deductibles and copayments.
- Silver Plans: These plans offer a balance between premium costs and coverage levels, with lower deductibles and copayments than Bronze plans.
- Gold Plans: These plans offer higher coverage levels, with lower deductibles and copayments than Silver plans, but also have higher premiums.
- Platinum Plans: These plans have the highest coverage levels, with the lowest deductibles and copayments, but also have the highest premiums.
Enrollment and Administration
Enrolling in a BCBS health insurance plan and managing your coverage involves a series of steps and processes. Understanding these processes ensures a smooth transition into your plan and provides you with the necessary tools to navigate your coverage effectively.
Enrollment Process
BCBS offers multiple enrollment options, allowing individuals and families to choose the best path for their needs.
- Through an Employer: Many employers offer BCBS plans as a benefit to their employees. Enrollment typically occurs during open enrollment periods or when an employee joins the company.
- Directly from BCBS: Individuals can purchase BCBS plans directly from the insurer, either online or through a licensed agent. This option provides flexibility for those not covered through an employer.
- Through the Marketplace: The Affordable Care Act (ACA) Marketplace provides a platform for individuals to compare and enroll in various health insurance plans, including BCBS offerings.
Customer Service and Support
BCBS prioritizes customer service and provides various channels to access assistance.
- Online Portal: BCBS members can access their account information, manage their plan, and submit claims through a secure online portal.
- Phone Support: BCBS offers 24/7 customer service via phone, allowing members to reach a representative for immediate assistance.
- Email: Members can contact BCBS via email for inquiries or concerns regarding their plan.
- Live Chat: Some BCBS websites offer live chat functionality, providing real-time assistance for specific questions.
Administrative Processes
BCBS utilizes various administrative processes to manage its plans efficiently, ensuring members receive the necessary support and coverage.
Claims Processing
Claims processing is a crucial part of the administrative process, involving the review and approval of medical bills submitted by members.
- Submitting Claims: Members can submit claims electronically through the online portal, by mail, or via fax.
- Claim Review: BCBS reviews claims for eligibility and coverage based on the plan’s terms and conditions.
- Payment Processing: Approved claims are processed, and payments are typically sent directly to the provider or member.
Appeals Process
Members have the right to appeal claim denials or coverage decisions.
- Appeal Request: Members can submit an appeal request in writing, outlining the reasons for their disagreement.
- Review Process: BCBS reviews the appeal and provides a decision within a specified timeframe.
- External Review: If the appeal is denied, members may have the option to seek an external review by an independent entity.
Consumer Considerations
Choosing the right BCBS health insurance plan can be a significant decision, as it directly impacts your healthcare access, financial stability, and overall well-being. This section will guide you through key factors to consider when selecting a plan, enabling you to make an informed choice that aligns with your individual needs and circumstances.
Understanding Your Health Needs
Before exploring BCBS plans, it’s crucial to assess your individual health needs. Consider your current health status, any pre-existing conditions, and anticipated healthcare requirements. This will help you prioritize coverage that addresses your specific needs. For instance, if you have a chronic condition like diabetes or asthma, you’ll need a plan with comprehensive coverage for medications, treatments, and specialist visits.
Budget Considerations
Your budget is another crucial factor. BCBS offers a range of plans with varying premiums, deductibles, and copayments. It’s important to determine your budget constraints and choose a plan that fits your financial situation. For example, if you’re on a tight budget, you may opt for a high-deductible plan with a lower premium, but be prepared to pay more out-of-pocket for healthcare services.
Lifestyle and Coverage
Your lifestyle also influences your insurance needs. If you’re a frequent traveler, consider plans with international coverage. If you have a family, look for plans that include dependents. Additionally, evaluate the plan’s network and provider access to ensure you have convenient access to healthcare services in your area.
Comparing BCBS Plans
Once you’ve considered your health needs, budget, and lifestyle, it’s time to compare different BCBS plans. You can use online comparison tools or consult with a broker to evaluate various plans and their features. Key factors to compare include:
- Premium: The monthly cost of your insurance plan.
- Deductible: The amount you pay out-of-pocket before your insurance coverage kicks in.
- Copayment: The fixed amount you pay for specific services, such as doctor’s visits or prescriptions.
- Coinsurance: The percentage of the cost you pay after your deductible is met.
- Network: The list of doctors, hospitals, and other healthcare providers that are covered by your plan.
- Benefits: The specific services and treatments covered by your plan.
Reviewing the BCBS Plan Document
Before enrolling in any BCBS plan, it’s crucial to read and understand the plan document. This document Artikels all the details of your coverage, including benefits, limitations, and exclusions. It’s important to review this document thoroughly to ensure you fully understand the terms and conditions of your plan.
Future Trends in BCBS
The healthcare insurance landscape is constantly evolving, driven by technological advancements, changing demographics, and evolving consumer preferences. These trends are shaping the future of BCBS plans, prompting the organization to adapt and innovate to remain competitive and meet the evolving needs of its members.
Impact of Technology and Innovation
The integration of technology is revolutionizing the healthcare insurance industry, influencing the way BCBS operates and interacts with its members.
- Telehealth and Virtual Care: The rise of telehealth and virtual care is transforming healthcare delivery, providing patients with convenient access to medical services from the comfort of their homes. BCBS is actively embracing telehealth by expanding its coverage to include virtual consultations and remote monitoring, enhancing the accessibility and affordability of healthcare for its members.
- Data Analytics and Predictive Modeling: Advancements in data analytics and predictive modeling enable BCBS to better understand the health needs of its members, identify potential health risks, and develop targeted interventions. This data-driven approach helps personalize healthcare plans, optimize care delivery, and reduce healthcare costs.
- Artificial Intelligence (AI) and Machine Learning: AI and machine learning are playing an increasingly important role in healthcare insurance, streamlining administrative processes, automating tasks, and improving claims processing efficiency. BCBS is exploring the use of AI to personalize health recommendations, detect fraud, and enhance customer service.
Final Review
Choosing the right BCBS health insurance plan requires a thoughtful assessment of individual needs, budget, and lifestyle. Understanding the nuances of coverage, network access, and administrative processes is crucial for making informed decisions. By navigating the complexities of BCBS plans, consumers can secure comprehensive healthcare coverage that aligns with their unique circumstances. The future of healthcare is evolving rapidly, and BCBS is at the forefront of this transformation, continuously adapting its offerings to meet the changing needs of its members. As technology and innovation continue to shape the industry, BCBS remains a key player in providing accessible and affordable healthcare solutions for millions of Americans.